At What Age Do Migraines Stop?
The tendency to have Migraine relates to inheritance of the Migraine gene from one’s family. Migraine is said to be genetic and familial in causation. Although the attacks usually start in teens or early twenties, some persons do not start Migraine headaches till later in life.
This is an article by Britt Talley Daniel MD, member of the American Academy of Neurology, migraine textbook author, podcaster, YouTube video producer, and blogger.
For persons living with Migraine it would be helpful to know how long they usually continue, that is when do they stop?
Check out my eBook on Migraine here.
Migraine generally stops for women at age 65-70. Migraine stops for men at age 50-60 years old. A small percentage of persons (2-5%) continue having Migraine past 80 years old.
Some women stop their Migraines after menopause which has an average age of onset at 51. Occasional persons only have Migraine headaches for months to a year in mid-life and then they stop.
Lipton RB , Stewart WF. Neurology.1993;43 (suppl3): S6-10.
Related questions
What is the usual age Migraine stops for women?
To discuss this question, it is helpful to note that the International Classification of Headache Disorders 3 lists 4 different types of Migraine and these types of Migraine stop at different times:
Migraine without aura
Migraine with aura
Menstrually related Migraine with or without aura
Pure Menstrual Migraine.
This differentiation is important because Migraine that comes with menstruation usually gets better after menopause, while non-estrogen related Migraine may not.
It can be helpful to see the effect of estrogen on a woman’s Migraine pattern by asking if she had reduced Migraines previously during her pregnancies. Migraine improvement during pregnancy may relate to decreased headaches after menopause.
The average age of onset of menopause is 51 but it can be in the 40’or 50’s. Menopause is defined as having 12 months with no menstrual period.
If a woman with Pure Menstrual Migraine or Menstrually related Migraine had few Migraines during previous pregnancies, she may well end her Migraine experience at the time of her Menopause.
For these women Migraine may end at menopause. About 60% of women with Migraine have either Pure Menstrual Migraine or Menstrually related Migraine.
The other 40% of women may note their Migraines ending at their age of 50 or 60years old.
Menstrual Cycle
What about perimenopause and Migraine for women?
Many women start the perimenopausal phase of their menstrual cycle in their late forties. Perimenopause means “around the time of menopause” and can last for 8 to 10 years. Estrogen and progesterone production becomes more irregular with a decrease in the amounts of hormones made along with irregular production.
Women may have an increase in frequency and intensity of their Migraine headaches during perimenopause, making this time in their lives accompanied by some of their worse Migraines. Some women have the onset of their first attacks of Migraine during perimenopause.
Perimenopause can be a difficult time with irregular menstrual flow times, hot flashes, vaginal dryness, mood changes, and trouble sleeping. Along with these common physical changes women may experience an increase in Migraine intensity and frequency.
There is a decrease in the amount of secreted estrogen during menopause due to pituitary induced decline in the neurotransmitter, serotonin, in the brain. There also is an increase in prostaglandin release during this time. All these changes can really affect the 70% of women who have Migraines with their menstrual cycle.
Perimenopause may result in interrupted sleep, a known Migraine aggravator. However not every woman has worse Migraines during perimenopause, some have an increase, some find no change.
What is the effect of menopause on Migraine?
Only several studies have looked at this and they have shown that:
The menopause makes migraine worse for up to 45% of women.
30-45% do not notice a difference.
15% notice an improvement.
Migraine attacks for some continue to follow a cyclical pattern years after the menopause and the reason for this is unclear.
At what age does Migraine stop for men?
Forty percent of persons with Migraine lose their attacks by age 65 and this affects Men also who usually lose their Migraine attacks starting in their fifties and sixties.
Does Migraine get worse in adults?
Migraine attacks do often become more frequent and more intense with ageing. Migraine often gets worse in adults. Headache diaries studied over decades show an increase in the number of “Migraine headache days” as time goes by.
This increase in Migraine coincides with the transformation from episodic (14 or less Migraines/month) into chronic Migraine (15 or more Migraines/month 8 of which have Migraine features) due to medication overuse syndrome.
Increased Migraines during adulthood may relate to the risk factors of stress, anxiety, overweight, head injury, fibromyalgia, and depression. 50% of persons may also be depressed and 40% have generalized anxiety disorder.
Are there changes in the brain of persons with Migraine as they age?
Migraine can cause an increased number of T2 microvascular lesions and silent brain infarctions (strokes). These are referred to casually as “spots or white dots and specifically as WMA’s (White Matter Abnormalities) or T2 microvascular lesions. There also may be larger lesions consistent with brain damage or infarction.
The incidence of T2 lesions is: Migraine with aura: 8.1%, Migraine without aura: 2.2%
Brain infarction occurs far more frequently than expected in Migraine patients. This is increased in Migraine with aura female patients, 8% of whom have subclinical cerebellar infarcts. These lesions are usually clinically silent.
It is thought that a causal relationship between Migraine severity and lesion load exists, but no studies have shown these T2 lesions have relevant long-term functional correlates.
As far as is currently known these T2 microvascular lesions are not associated with increased risk of stroke or cognitive loss and have no serious pathological significance although this position may change with future research.
Use of preventive medication, triptan acute therapy, and living the Migraine lifestyle are important components of the treatment of such patients.
Microvascular T2 lesions with Migraine
What about the occurrence of acephalic Migraine?
Acephalic Migraine is also known as Migraine aura without headache, amigrainous Migraine, isolated visual Migraine, and optical Migraine. Sometimes it just occurs in men, but more frequently it occurs in middle-aged women.
It usually consists of a typical Migraine with aura visual event with seeing spots, holes, flashing lights, or zig zag lines which usually last minutes but which come without any headache. There may also be nausea, numbness, and photophobia.
On interview many of these patients who are usually women, aged 65 or so deny any previous historical links to Migraine. Yet they may have experienced Migraine aliases like menstrual headache, hungry headache, nocturnal headache, sinus headache, or motion sickness earlier in life.
Persons with acephalic Migraine stop their attacks at the same time as regular Migraine as discussed in this article.
Zig Zag Migraine visual image, enlarging from a to e.
What is a common provoking habit of elderly persons with Migraine?
A common issue here and likely the most common reason that elderly migraineurs see a headache doctor is overtreating their headaches and developing medication overuse headache. It is reported that 1/3 of elderly Migraine patients are over treating.
Overtreating Migraine gives you chronic Migraine
What about persons with abdominal Migraine?
Abdominal Migraine is mainly GI symptoms of nausea, vomiting, stomach cramping, anorexia, and centrally positioned pain around the umbilicus. There may be mild headache, but GI symptoms are more prominent.
Abdominal Migraine starts between 11 and 20 years old and in 70% of persons turns into plain old Migraine headaches by 20 years old. Girls outnumber involved boys by 3 to 1. However, for this population of children, Migraine starts at a much younger age.
Child with abdominal Migraine vomiting
Treatment options for persons with Migraine that may end the headaches.
Lifestyle for living with Migraine.
Attention to these lifestyle issues can significantly improve or sometimes stop the occurrence of Migraine attacks.
Caffeine is a double-edged sword.
Most persons like to drink caffeine and although it is an addictive drug according to the Diagnostic and Statistical Manual of Mental Disorders V, drinking caffeine can be a very pleasant experience for most people.
The problem is that caffeine is a vasoconstrictor and can aggravate Migraine or give medication overuse headache if too much is used. This issue is especially important to persons with Migraine.
The American Headache Society has stated that caffeine is the number one drug in America causing an increase in the intensity and frequency of migraine. Caffeine use is confusing because many persons know that caffeine may be used to treat headache, but they need to learn that if taken frequently, more than 2 days a week, it can cause medication overuse headache, previously called--rebound headache.
As a neurologist and headache doctor I know that many people with Migraine do drink some caffeine and they get by with it and probably do ok, but it is the slow, sneaky addictive quality of the drug that bothers me as a doctor, and I think bothers many Migraine patients.
Overall, I advise Migraine patients to not drink caffeine.
Coffee, coffee, coffee, Oh, I need more coffee!
Diet issues.
Avoid fasting or missing a meal.
A small breakfast will suffice, but usually for mostly young women, who fill the offices of neurologic headache doctors all over the world, the advice to eat breakfast will be met by a vacant look and denial many times.
Did you know that the word “breakfast: means “to break the fasting of sleep.” If you do not eat and without your knowing it, your pituitary gland will sense your low blood sugar and send out a hormonal signal that will cause vasodilatation of your cerebral arteries and start your “hungry headache” migraine.
Three meals a day is advised by all medically accepted weight loss programs (Jenny Craig/Weightwatchers), but my experience is that most mothers will feed their children three meals a day but not themselves.
No time to sit and eat today; I’ve got to work and work. No play!
Exercise.
The American Heart Association has recommendations for Adults and here it is straight copy and paste from the AHA website.
Recommendations for Adults
Get at least 150 minutes per week of moderate-intensity aerobic activity or 75 minutes per week of vigorous aerobic activity, or a combination of both, preferably spread throughout the week.
Add moderate- to high-intensity muscle-strengthening activity (such as resistance or weights) on at least 2 days per week.
Spend less time sitting. Even light-intensity activity can offset some of the risks of being sedentary.
Gain even more benefits by being active at least 300 minutes (5 hours) per week.
Increase amount and intensity gradually over time.
The above are recommendations for general health, but did you know that one may improve migraine, anxiety/panic disorder, depression, tension headache, and sleep problems with aerobic exercise?
There are hundreds of scientific articles over the past 20 years proving that exercise works for headache therapy. Aerobic exercise is: dance aerobics, jogging, cycling, swimming, rowing, cross-country skiing, and stair-stepping.
It is not walking, lifting weights alone, stretching, or playing most games, like tennis or racquetball. If you are already exercising and still have bad headaches, consider increasing your exercise program.
Exercise is something you can do for yourself to take control of your headaches. It takes determination, time, and effort.
Overweight can increase the frequency of Migraine attacks.
Some migraine patients get a “work-out headache” if they get hot. If this happens to you then try to work out so you do not get so hot. Exercise in front of a fan or in air conditioning.
Take ibuprofen, Excedrin, or a half of a Triptan drug before you work out, remembering to limit all painkillers and triptans to no more than 2 days per week.
If you still get a work-out headache, then try swimming.
Here we go…2,3,4. Very good 2,3,4.
Adequate Sleep.
Migraine persons often do not sleep well. 50% of Migraine patients are depressed or 40% have GAD (generalized anxiety disorder) which both have insomnia as one of the cardinal symptoms.
Regulate your sleep. Set your sleep/wake cycle to rise and go to sleep at the same time every day-even through the weekend. Adults should sleep between 7 to 8 hours every night.
Wake up the same time on Saturday and Sunday mornings as you do during the rest of the week.
Migraine may be treated by sleep RESTRICTION. Avoid oversleeping Saturday morning or falling asleep for that seductive two-hour nap on Sunday afternoon. Set an alarm for 15-20 minutes for a short, energy restoring nap. If you never learned how to take a short nap, then learn. It can be done.
There are stages of sleep. Most persons with Migraine only get to a light stage of sleep at night, not deep sleep. Too much sleep or not enough sleep can set off a Migraine.
Unwind at the end of the day. Listen to soothing music, take a warm bath, read a favorite book.
Hard exercise, big meals, caffeine, nicotine, and alcohol can interfere with sleep.
Minimize distractions. Save your bedroom for sleep and intimate relations. Do not watch television or take work materials to bed. Close your bedroom door. Use a fan to muffle distracting noises.
Be sure that none of your medications can interfere with sleep. Look up drug side effects on the internet.
1 sheep, 2 sheep, 3 sheep, sheesh! I can’t sleep.
Dealing with Stress
Many patients I talk with deny having any stress. Talking with them is like “It’s somebody else’s problem, not mine.” They either don’t understand what stress is or are willing to discuss it with a “regular, non- psychiatric doctor.
These are the stressful events in life:
Change of environment-leaving home to go to school or start a new job.
Death, accident, or major illness of a parent, grandparent, sibling, close friend, spouse, or sweetheart.
Birth of a new child.
Loss of a job; starting a new job.
Financial stress, mortgages due, old bills, unexpected financial responsibilities.
We all go through these types of things. They are the ebb and flow of our lives.
Therefore, learn to talk over your daily life problems with your friends, family, preacher, priest, or rabbi.
Develop a support system to sustain you in life, built up of key people that are there for you when you need them.
Plan time to relax and spend on hobbies or interests. Normal people have hobbies which is something you do for fun and relaxation, that is creative and not goal or money-making oriented. Children and family are not hobbies. Please look up the word “hobby” in the dictionary if you think this.
Turn off that cell phone, computer, or iPad and get a life. Plan three-day weekends several times a year rather than one two-week holiday in August. Leave that depressing, stressful job, or get counseling and try to change a personal relationship that is causing problems.
Try avoiding deep breathing, get family or personal counseling, or learn CBT—cognitive behavioral counselling. Look up CBT on the internet.
Cannot handle Pressure!
Avoid Overtreatment with Medication.
Do not take too much caffeine, over the counter drugs, triptans, or painkillers for headache. In general, all migraine patients should limit all such drugs to no more than 2 days per week.
The migraine process generates neurochemicals which are released in the brain and that inflame the thalamus, trigeminal nerve, and cerebral arteries. These neurochemicals stay in the body 3 days and once they inflame the brain they are repeatedly released every time other pain killers, caffeine, Advil, Tylenol are consumed, starting a process of continuous headache.
I once saw a man who told me he had been taking 10 Excedrin migraine pills for over fifty years (10 X 65= 650 mg/day) and he had a headache all that time until I convinced him to stop Excedrin. Then his headaches cleared up.
There is no data that opioid narcotics help migraine headache, they just cause problems and should not be used for “rescue treatment.” The U.S. is now going through a change in the use of opioid narcotics and barbiturate drugs since they cause people to die in their sleep, are addictive, and cause medication overuse headache.
Narcotics should be used never or only for persons who are in severe pain and near the end of life, for acute trauma, or surgery, only for a short time and then stopped. Death from opioid narcotics is a top problem now in America.
Butalbital found in Fiorinal, Fioricett, and Esgic has been banned in every country in the world except Canada and the U.S. because it causes medication overuse headache. The word “narcotic” comes from the Greek word that means “sleep.” In Texas, the number one reason for the State Medical Board to restrict physicians concerns their use of opioid medications and more licenses are restricted or revoked regarding this issue than any other.
Hey, call in my refill of Fiorinal to Walgreens, okay?
Avoid Food Triggers.
People with Migraine may have their own individual foods that seem to set off their headaches and the subject of food triggers is a controversial, still poorly researched subject.
Common food triggers are: alcohol, chocolate, aged cheeses, MSG, and red wine. If you know certain foods are a problem for you, do not eat them.
See my article on Food-Triggered Migraine at www.doctormigraine.com.
Eat regular, balanced meals. Basing your diet primarily on fruits, vegetables, whole grains, lean protein, and healthy fats (and limiting foods that trigger an attack) is a good way to prevent migraines and/or headaches. Also, do not skip meals. Skipping meals makes you hungry, which can trigger a migraine.
Avoid all your known Migraine Triggers.
Migraine triggers may be:
Stress 79.7%
Hormones (in women) 65.1%
Not eating 57.3%
Weather 53.2%
Sleep disturbance 49.8%
Perfume or odor 43.7%
Neck pain 8.4%
Light (s) glare 38.1%
Alcohol 37.8%
Smoke 35.7%
Sleeping late 32.0%
Heat 30.3%
Food 26.9%
Exercise 22.1%
Sexual activity 5.2%
Reference. Kelman writing in Cephalalgia in 2007 on “The triggers or precipitants of the acute migraine attack.”
Check Barometric Pressure changes aggravating Migraine.
There are scientific articles verifying Migraine attacks with changes in barometric pressure. I think this has been established the reason for the attacks and how pressure affects the brain is not understood.
Modern cell phones or computers can report current barometric pressure changes for where you live. If you get attacks with barometric pressure changes, then keep a pressure diary and watch out for a Migraine that may occur then. Migraineurs may pretreat with a triptan for some attacks.
What to do when a Migraine does start.
Treat early with a Triptan when a Migraine starts. Find a cool, dark, quiet space. Get off TV or your cell phone. Rest your eyes.
Relax. Deep breathing from your diaphragm can help you relax. Focus on inhaling and exhaling slowly.
Think positively. Learn how to deal with a Migraine interrupting your day. Learn CBT skills. “It’s not the end of the world.”
Keep a migraine diary.
There are a number of free cell phone apps for migraine. I have a blog post on the subject at www.doctormigraine.com.
Patients can plot life issues—menstruation, weather change, stress, missed meals, occurrence at night or a “wake up headache.”
Study carefully any trigger that seems important and recurrent. Living with migraines is a daily challenge but making healthy lifestyle choices can help. Ask your friends and loved ones for support. Pray to God for help with your life and your health.
Triptans for Acute Migraine Treatment
I tell patients that triptans have "headache free" data for migraine treatment in 70-80% of patients. Patients may be headache free by 2 hours if they treat with a triptan at onset of their migraine. DHE has no headache free data but Migranal nasal spray may provide relief in 61% of migraine patients at 2 hours if used at onset.
Many migraine patients use over the counter drugs such as supplements, caffeine, NSAIDS like Aleve and Advil, or doctor prescription prescribed narcotics like hydrocodone, and butalbital.
These drugs provide a variable clinical response, and narcotics should not be used for migraine and lead straight into medication overuse headache.
But insurance cover for triptans is spotty and some patients do not respond or have limiting medical issues so they cannot take them.
Triptans for Migraine Treatment. Triptans are the first choice for acute migraine treatment. They are recommended by migraine headache authorities and they are all generic and reasonably priced with insurance.
Injectable sumatriptan 6 mg subcutaneous is the best all round drug because it works in 10 minutes and gives the highest dose in the brain of medication-100 mg.
What is the triptan response rate?
About 20% of patients do not respond to triptans or have a contraindication like previous heart attack, coronary artery disease, or out of control hypertension.
Modern treatment for migraine patients should be a trial of one or more of the triptans, the doctor adjusting the dose or trying a new drug on the follow-up clinic visit.
What is the best treatment dose?
Patients should always be advised to treat at onset and trying different doses, using a low dose to high dose mind set.
What is insurance coverage of Triptans like?
There are 7 triptans and they all are generic now and it is doubtful more will be made. Insurance coverage of triptans should not be an issue, but it is a big issue in headache practice since insurance companies have different “tiers” of drugs.
Their tier 1 drug will be cheaper for the patient and represents a financial deal they have made with pharmaceutical providers, but it is a deal that has nothing to do with the reasonable practice of medicine where the doctor, reading the literature and using his practice experience, tries to make the best drug decision for a patient.
The rarely used triptans now are Amerge (naratriptan) and Axert (almotriptan). Naratriptan onset is 1-2 hours, as is Frovatriptan, but Frovatriptan lasts the longest of any triptan—26 hours, so it has a special place in treating menstrual migraine.
What is the best triptan?
This question has never been answered. Imitrex (sumatriptan) was the first and has always been the most popular drug and it comes in more applications—Sub Cutaneous, 2 forms of Nasal Spray, 3 different sized oral pills, and mixed with naproxen.
Frova (frovatriptan) has a special place in treating menstrual migraine. The other short onset triptans—Maxalt (rizatriptan), Zomig (zolmitriptan), and Relpax (eletriptan) are commonly used and effective.
The generic short onset triptans have an onset of 30 minutes while name brand Imitrex, and Treximet both work in 15 minutes. Time of treatment is a big deal in the migraine world, but few patients want to pay for name brand Imitrex or take the shot because of rejection of needles.
The question of “Which is the best triptan?” could only be answered by a large drug trial using all the drugs and seeing who wins. But now all the drugs are generic and insurance companies would have to pay for the study it will never be done.
Imitrex (sumatriptan) has a duration of 2 hours, while Relpax (eletriptan) is advertised for its long duration of 6 hours. No journal on headache or article ever named the best drug, until years ago when the American Academy of Neurology headache group broke the ice and reported the best drug overall, and it was no surprise; they named injectable SC Imitrex (sumatriptan) 6 mg as the best triptan, the first and now the best.
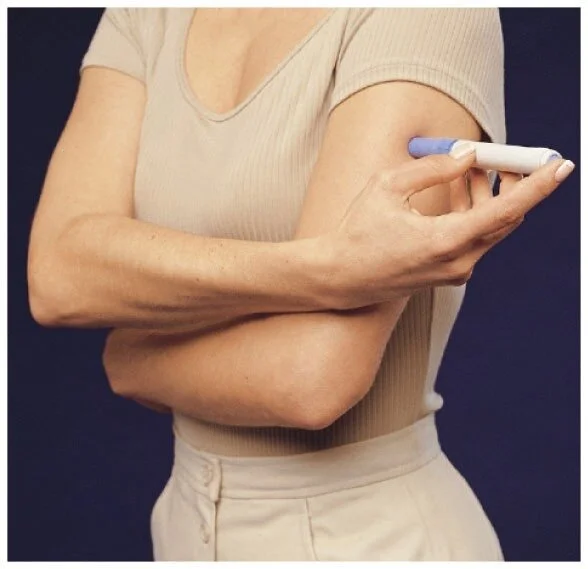
Sumatriptan injection
Data I have seen on Imitrex (and I do not know if for other triptans), is that Imitrex (sumatriptan) SC 6 mg works in 10 minutes and gives a level in the brain of 100 mg. Nasal spray Imitrex (sumatriptan) works in 10 minutes and gives a brain level of 10 mg. Oral tablet form sumatriptan works in 30 minutes and gives a brain level of 30 mg.
No surprise here, nasal sprays give low drug levels. So, injectable Imitrex (sumatriptan) works 3 times faster than oral and gives a blood level that is 3 times higher. Glaxo, the drug firm that brought out injectable Imitrex, put their money on the sure winner—injectable SC Imitrex.
The original Glaxo drug trial for the FDA looked at 6 mg, 4 mg, and 3 mg doses and they all are available now and work well, with decreasing incidence of side effects according to dose.
For the needle shy there is pressure jet 6 mg DosePro which is a system that drives sumatriptan through the skin and into the body.
A final triptan comment is that when Glaxo’s name brand Imitrex ran out they brought out Treximet which is a combo drug of sumatriptan and naproxen. Glaxo got Treximet through the FDA because for some migraine patients, it worked better than Imitrex alone.
Naproxen lasts 12 hours and is an NSAID. After Treximet came out naproxen was tried with all the other oral triptans and found to work better for some patients. I generally ask the patient to just try the triptan first alone, but if they are not satisfied to next try it with 2 Aleve which is 400 mg of naproxen.
Are there any new acute therapy migraine drugs?
There are several new drugs for acute migraine treatment available in 2020. And they are:
Nurtec (Rimegepant)
Ubrelvy (Ubrogepant)
Reyvow (Lasmiditan)
How well do the new drugs work?
How well do these drugs work in comparison with triptans? These 3 drugs decrease symptoms of migraine attacks and improve function compared with placebo. They may be helpful for the 20% of patients who are unable to take triptans.
How do these new drugs work?
They are all oral drugs. Nurtec and Ubrelvy blocks the CGRP receptor. CGRP is one of the inflammatory neurochemicals released by the migraine process.
Reyvow works on 5HT 1E receptors which inhibit trigeminal nerve pain pathways. Reyvow also inhibits release of neurotransmitters and neuropeptides.
Reyvow does not cause arterial vasoconstriction like triptans do and can be used in patients with heart disease, stroke, and hypertension.
What is the expense of these new drugs?
Both sumatriptan and eletriptan are less expensive and more effective than the newer agents.
Nurtec (Rimegepant) is administered as a fast acting orally disintegrating single dosed 75 mg tablet in patients with episodic or chronic migraine. The study demonstrated a statistically significant reduction from baseline in monthly migraine days in individuals treated with rimegepant compared with placebo.
Treatment provided pain relief within 1 hour. Nurtec (Rimegepant) had a sustained efficacy of pain relief lasting as long as 48 hours for many patients.
This is an unusual drug that works quickly for acute therapy, but also has been approved for episodic and chronic migraine prevention.
Ubrelvy (Ubrogepant) 20% of patients who received 50 or 100 mg of Ubrogepant orally had freedom from headache pain at 2 hours. The FDA approved Ubrelvy (Ubrogepant) for acute treatment of migraine.
Ubrelvy (Ubrogepant) has no effect of vasoconstriction and is okay with heart or stroke conditions.
Reyvow (Lasmiditan) is the first and only Ditan for the acute treatment of migraine with or without aura. Reyvow (lasmiditan) is not indicated for the preventive treatment of migraine.
Dosing Three oral dose sizes of Reyvow (lasmiditan) exist-50, 100, and 200 mg. Only 1 dose should be taken in 24 hours.
A single dose of Reyvow (lasmiditan) may cause significant driving impairment due to increased sleepiness lasting as long as 8 hours.
Therefore, because of this possible side effect patients are advised to not perform potentially hazardous activities requiring complete mental alertness, such as driving a motor vehicle or operating machinery for at least 8 hours after each dose of Reyvow (lasmiditan).
Rimegepant and Ubrogepant both block CGRP activity while Lasmiditan is a serotonin (5-HT) 1F receptor agonist.
All migraine patients who do not respond well to triptans, and that is about 20% of patients, should discuss these new drugs with their neurologists.
Preventive treatment
American Academy of Neurology advice for Migraine preventive treatment.
Level A drugs, that is those which have been established as effective, are:
Divalproex sodium, sodium valproate 400-1000 mg/day
Topamax (topiramate), short acting, or Trokendia XR, Qudexy XR, long acting 25-200 mg/day.
Frovatriptan (long acting triptan--26 hours) for menstrually related migraine short term 2.5 mg/day
Onabotulinumtoxin A (Botox)--physician injects onabotulinumtoxin A into the muscles of the forehead and neck. When effective, the treatment is repeated every 3 months. Indicated by the FDA for persons with Chronic Migraine (15 headache days/month, 8 of which are like migraine).
Botox has been found to be only modestly effective for preventing migraines in the most frequent suffers. Botox prevented 1.8 headaches a month more than placebo.
Betablockers
Metoprolol 47.5-200 mg/day
propranolol 120-240 mg/day
Timolol 10-15 mg bid
Level B drugs, those which are “probably effective.”
Amitriptyline 25-150 mg/day
nortriptyline 25-50 mg/day
venlafaxine 150 mg extended release/day
Level C drugs, thought to be “possibly effective.”
ACE inhibitors (lisinopril) 10-20 mg/day
angiotensin receptor blockers (candesartan) 16 mg/day
alpha-agonists (clonidine) 0.75-0.15 mg/day; patch formulations also studied.
carbamazepine 600 mg/day
Cyproheptadine 4 mg/day
Atenolol 100 mg/day
Guanfacine 0.5-1 mg/day
3 Special considerations
All the A listed drugs above for prevention may reduce headache by 30-40%. However, there are special considerations for patients with multiple medical problems using these drugs.
Patients who are anxious and cannot sleep or have depression may be given amitriptyline or nortriptyline. Amitriptyline is also the go to drug for patients who have limited funds or no insurance drug coverage since it is so cheap, often just 3-4 dollars a month.
Persons who have epilepsy and migraine and overweight should be offered topiramate, but this drug should not be given to patients with a history of kidney stones.
Patients with tremor, hypertension, or migraine may be given a beta blocker which may treat all three conditions.
Thinking this way, the doctor and the patient may get a double treatment effect from a single preventive medication.
Also, there is no endorsement by the American Academy of Neurology or the American Headache Society on the new CGRP drugs—Aimovig, Ajovy, Vyepti, or Emgality--for migraine prevention, but it is well known that these new drugs work better than the old-time preventive drugs listed above.
CGRP drugs reduce Migraine 50% in 50% of patients, by 75% in 25% of patients, and by 100% in 25%. These are amazing results for the CGRP drugs which have significantly changed the experience of having Migraine for my persons.
The CGRP antibodies have had an impressive impact on Migraine Prevention. The CGRP antibodies interact with other drugs well and have few side effects.
All the CGRP Monoclonals inhibit signaling by calcitonin gene-related peptide (CGRP). In general, they all performed similarly, both in efficacy and in safety and tolerability.
All the new drugs except Vyepti are administered subcutaneously in the thigh or abdomen while Vyepti is given intravenously. The drugs are given every 1 to 3 months.
Aimovig, a CGRP preventive drug for Migraine
What is the usual age of onset of Migraine?
Migraine usually starts at 25 to 30 for men and women with peak occurrence between ages 30-39 For some Migraine starts in the late teens or early twenties. Women have Migraine more frequently than men at a rate of 3/1 starting as teenagers, and this incidence continues with ageing.
85% of adults with Migraine are women. Hormones are thought to be one of the main contributing factors to the increased occurrence of Migraine in women.
Occasional patients start with regular Migraine during childhood at a young age of 5 or 6 years old. Migraine at onset during childhood may not have a genetic or familial cause of origin.
Some persons develop Migraine as adults, particularly women around perimenopause, which is the period of time before menopause. Ninety percent of persons with Migraine have their first attack before 40 years old.
Check out my big book on Migraine here.
This site is owned and operated by Internet School LLC, a limited liability company headquartered in Dallas, Texas, USA. Internet School LLC is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. Although this site provides information about various medical conditions, the reader is directed to his own treating physician for medical treatment.
Follow me at: www.doctormigraine.com, Pinterest, Amazon books, Podcasts, and YouTube.
All the best.
Britt Talley Daniel MD