Menstrual Migraine Symptoms and Treatment.
Migraine has an incidence of 12% and is present in 25% of women and 6% of men. For women migraine is their most frequent medical problem. In general Migraine is said to be genetic and 5 genes have been identified. Menstrual Migraine relates to the fall of estrogen during a normal monthly cycle or due to estrogen withdrawal the fourth week of a woman’s cycle while on the pill. The pill switches from 3 weeks of estrogen to progesterone for the fourth week.
For most women with Migraine their monthly menstrual Migraine headache is the worst, the longest, and the most difficult Migraine they get so that good treatment for menstrual Migraine is especially important.
Women need advice on how to manage these “special, difficult” Migraines.
This is an article by Britt Talley Daniel MD, retired member of the American Academy of Neurology, the American Headache Society, migraine textbook author, podcaster, YouTube video producer, and blogger.
Menstrual Migraine may be treated by adhering to a healthy Migraine lifestyle and treating early with an NSAID such as naproxen or ibuprofen or a short acting triptan such as sumatriptan, rizatriptan, or eletriptan, or use of a gepant such as Nurtec ODT (rimegepant).
Use these drugs for the 5-7 days when headache is severe during the cycle. Migraine patients with more frequent headache should consider using a preventive medication.
Related questions.
How is Menstrual Migraine defined?
Menstrually Related Migraine with or without Aura is defined by the International Classification of Headache Disorders, ICHD3, as migraine with or without aura that occurs 2 days before or 3 days after the onset of menstrual bleeding where menstrual onset was defined as day 1.
Menstrual migraine, also called catamenial migraine, is further divided into:
Pure Menstrual Migraine where migraine headaches only occur during the menstrual cycle. This occurs in 7-14% of women.
Menstrually Related Migraine With or Without Aura where the headaches occur at menstruation and at other times during the month as well. This is the most common type of menstrual Migraine and occurs in 50% of Migraineurs.
Does adherence to a Migraine lifestyle treat Menstrual Migraine?
In general women with migraine are encouraged to not ignore their cycle but instead plan for it. They are advised to relax their personal and work schedule during their cycle and to get lots of rest, exercise, and proper nutrition. This is important because menstrual migraines are more severe, last longer, and are more difficult to treat than the usual migraine.
The Migraine lifestyle is adequate eating, proper amount of sleep, exercise, limiting or eliminating caffeine, dealing with stress, and avoiding overtreating with medication. Other ideas are avoiding stress and food triggers and charting barometric pressure changes.
Lady jogging
Buy my Migraine Minibook on Amazon here.
What about keeping a diary or chart of Migraine and menstrual cycle occurrence?
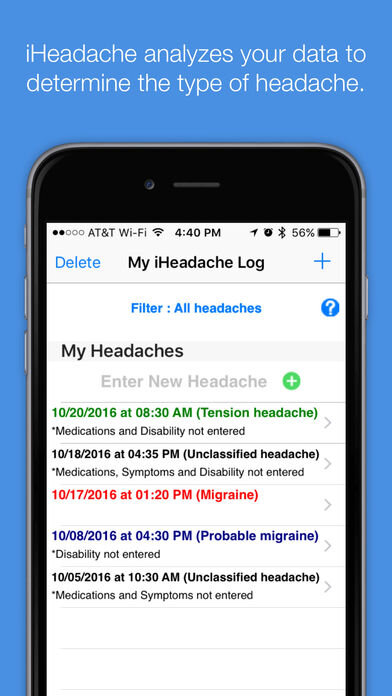
There are a number of free cell phone apps for keeping account of Migraines. Charting the occurrence of Migraine and the menstrual cycle for several months may help ensure an accurate diagnosis of Menstrually related Migraine.
The Menstrual Migraine Assessment Tool (MMAT)
This a simple questionnaire with three questions, that has shown to be fairly accurate in diagnosing menstrual migraine.
The three questions are:
Do migraines occur in the space of time 2 days before the beginning of a woman's period, until the third day after the start of the period? And does this happen in most months?
Do headaches that happen during this time become very severe?
Does the woman experience photophobia, which is a medical problem causing light to bother a person's eyes?
The answer to the first question has to be yes and there has to be at least one yes answer to either question 2 or question 3.
When to Treat Migraine Episodes.
Treat several days before, during, and after the menstrual cycle if the migraine doesn’t come consistently at the same time or if you have irregular periods. If the migraine usually comes the day before you bleed and you have regular periods, then start treating several days before bleeding.
A variety of drugs may be tried, and the following list is from simple, cheap, and few side effects to complicated, expensive, and possible side effects.
Simple Drugs to Try for Acute Therapy: Try over the counters like Tylenol (acetaminophen), Advil (ibuprofen), or Aleve (naproxen) taken as 1-2 X/day. Naproxen is used more often and lasts longer. Cambia is an NSAID approved for acute treatment of Migraine.
Dihydroergotamine (DHE) as injectable intramuscular DHE or nasal spray Migranal may be tried.
Timoptic (timolol) betablocker eye drops may be tried.
Triptans: oral Imitrex (sumatriptan) 100 mg, Zomig (zomatriptan) 2.5/5 mg, Maxalt (rizatriptan) 10mg, Axert (almotriptan) 12.5 mg, Relpax (eletriptan) 40 mg, Amerge (naratriptan) 2.5 mg, or Frova (frovatriptan) 2.5 mg, taken as 1-2 X/day.
Frova and Amerge are used for menstrual migraine due to their long half-life: Frova-26 hours, and Amerge-6 hours.
Frova, because of its long 26-hour half-life has become the drug with the most evidence as a short-term prophylactic agent for menstrual migraine. One Frova trial demonstrated that 57% of patients were migraine free over the course of 3 menstrual cycles.
The regimen used was 1 or 2 2.5 mg pills of Frovatriptan, twice daily, starting 2 days prior to the onset of menstruation, for a total of 6 days of treatment. With this regimen the patient can also take an additional 2.5 mg dose once a day for breakthrough headaches.
This treatment program was efficacious in women with pure menstrual migraine, and in select, difficult to treat women with migraines where previous abortive treatments had failed.
Because of this result, short-term prevention of menstrual migraine with frovatriptan has been given an A rating by the American Headache Society and the American Academy of Neurology for migraine prevention.
New Acute Treatment Drugs and Devices for Migraine 2020. Nurtec, Ubrelvy, and Reyvow are the first-of-a-kind medications in a new class of acute migraine treatments. Cefaly and GammaCore devices may be tried, but there is little data on all these forms of treatment. They should be considered for triptan failure patients.
Mini-Prevention Strategies
NSAIDs
NSAIDs taken twice a day during the 5-7 days surrounding the menstrual window may decrease or eliminate the menstrual migraine. Should the migraine occur during this time, it is likely to be less severe and becomes more amenable to treatment by a triptan.
Naproxen 550 mg dosed twice a day as mini prevention was shown to be effective when studied, and the benefit is believed to be a class effect, meaning that other NSAIDs are likely to give similar results.
Triptans
Multiple studies have been done with the acute medications typically used to treat usual migraines, but dosed continuously in the menstrual window, twice a day. This approach appears to decrease or eliminate menstrual migraine, although there are concerns that the migraines may be worse or become more frequent at other times of the month, possibly related to rebound or medication overuse. This would particularly be problematic in women who have frequent migraines throughout the month, as well as menstrual migraines.
The American Headache Society Evidence-based Guidelines rated frovatriptan as effective (Class A), and naratriptan and zolmitriptan as probably effective (Class B) for use in mini-prevention. However, the FDA did not feel the evidence of benefit for frovatriptan was sufficiently strong to approve it for this indication and has not given any triptan a recommended indication for mini prevention.
Triptan dosing for mini prevention is generally given twice daily. Either naratriptan 1 mg or zolmitriptan 2.5 mg dosed twice a day, or frovatriptan given with a starting dose of 10 mg, then 2.5 mg twice a day are typical regimens in the menstrual window that have studies backing their effective use.
NSAIDs, usually naproxen and a triptan taken together at the same time or as one pill as Treximet may also be used.
Preventive drugs for Menstrual Migraine Treatment.
Any of the group of drugs that may be used for prevention may work. They may be taken every day during the menstrual cycle or every day of the month. Data concerning the use of long-term preventive agents for menstrual migraine is sparse and the use of standard migraine preventive drugs is currently the most common form of therapy.
These drugs include Inderal (propranolol), Tenormin (atenolol), Topamax, Trokendia XR, or Quedexy XR (topiramate), and Elavil ((amitriptyline).
Depakote should not be used as it is completely contraindicated in menstruating females and has an X rated warning from the FDA regarding teratogenic damage to the fetus.
CGRP drugs Aimovig (erenumab), Vyepti (eptinezumab), Emgality (galcanezumab), Ajovy (fremanezumab), and Vyepti (Eptinezumab) are powerful new drugs for Migraine prevention that are given parentally every month or 3 months for Migraine prevention.
Estrogen: Many doctors prescribe estrogen-based birth control pills, estrogen IUDs, estrogen patches and pellets, and injections to persons with migraine. These drugs are all contraindicated for migraine by the FDA and can make the experience of migraine worse.
They are all relatively contraindicated by the FDA for patients with menstrually related migraine and migraine without aura, but they are absolutely contraindicated for women with migraine with aura for risk of stroke. Migraine with aura alone carries a 6 % risk of stroke.
Other problems are that estrogen treatment is called “a class 1 carcinogen” that is, a drug that may cause cancer. The incidence of breast cancer in 1960 before the pill came out was 6% but now it is 8%. The Mayo Clinic published an article stating there is a 6% risk of breast cancer in women.
Also, these estrogen treatments can cause an abortion by making cervical mucus thick so that an embryo can’t move down the tube and implant in the uterus. IUDs work by scraping an implanted embryo off the uterine wall, like a lawnmower cuts grass.
At this time additional data are needed to make specific recommendations regarding long-term prevention of therapy and menstrual migraine.
Warning regarding treatment of menstrual Migraine with estrogen drugs.
Elizabeth Loder published a book on menstrual migraine and is a Professor of Neurology at Harvard in Boston. She was chosen by the American Academy of Neurology to lead a team of neurologists investigating hormonal treatment of migraine with menses. These doctors reviewed the literature and then published the following article in the journal Headache.
Loder E, Rizzoli P, Golub J. Hormonal management of migraine associated with menses and the menopause: a clinical review. Headache. 2007;47(2):329-340.
Their summary statement is appended below.
”Hormonal treatment of migraine is not a first-line treatment strategy for most women with migraine. Evidence is lacking regarding its long-term harms and migraine is a contraindication to the use of exogenous estrogen in all women with aura and those aged 35 or older. The harm to benefit balances of several traditional non-hormonal therapies are better established.“
References:
1. Vetvik KG, Macgregor EA, Lundqvist C, Russell MB. Prevalence of menstrual migraine: a population-based study. Cephalalgia. 2013;34:280-288.
2. MacGregor EA, Victor TW, Hu X, et al. Characteristics of menstrual vs non-menstrual migraine: a post hoc, within-woman analysis of the usual-care phase of a nonrandomized menstrual migraine clinical trial. Headache. 2010;50:528-538.
3. Maasumi K, Tepper SJ, Kriegler J S. Menstrual migraine and treatment options: review. Headache. 2017;57;194-208.
4. Silberstein SD, Arthur EH, Schreiber C, Keywood C. A randomized trial of frovatriptan for the intermittent prevention of menstrual migraine. Neurol. 2004;63:261-269.
5. Silberstein SD, Berner T, Tobin J, Xiang Q, Campbell JC. Scheduled short-term prevention with frovatriptan for migraine occurring exclusively in association with menstruation. Headache. 2009;49:1283-1297.
6. Brandes J, Poole AC, Kallela M, et al. Short-term frovatriptan for the prevention of difficult-to-treat menstrual migraine attacks. Cephalalgia. 2009;29:1133-1148.
7. Newman LC, Lipton RB, Lay CL, Solomon S. A pilot study of oral sumatriptan as intermittent prophylaxis of menstruation-related migraine. Neurol. 1997;51:307-309.
8. Tuchman MM, Hee A, Emeribe U, Silberstein S. Oral zolmitriptan in the short-term prevention of menstrual migraine: a randomized, placebo-controlled study. CNS Drugs. 2008;22:877-886.
9. Newman L, Mannix LK, Landy S, et al. Naratriptan as short-term prophylaxis of menstrually associated migraine: a randomized, double-blind, placebo-controlled study. Headache. 2001;41:248-256.
10. Coffee, AL, Sulak PJ, Hill AJ, et al. Extended cycle combined oral contraceptives and prophylactic frovatriptan during the hormone-free interval in women with menstrual-related migraines. J Womens Health (Larchmt). 2014;23:310-317.
11. Sulak P, Willis S, Kuel T, et al. Headaches and oral contraceptives: impact of eliminating the standard 7-day placebo interval. Headache. 2007;47:27-37.
12. Hullett, PW, Maasumi, K Neurology Times Tuesday, Octoeber 17, 2017
Please stay on YouTube and watch my other articles to learn about migraine.
This is a post by Britt Talley Daniel MD, member of the American Academy of Neurology, the American Headache Society, migraine textbook author, and blogger.
Check out my books on Migraine on Amazon.
Follow my webpage at www.doctormigraine.com.
Titles: Migraine-400-page textbook, and Volume 1 of the Mini Neurology Series, Migraine-40-page book. Both books are offered as print or eBooks.
All the best.
Follow me at: www.doctormigraine.com, Pinterest, Amazon books, Podbean, and YouTube.
Britt Talley Daniel MD
P.S. Okay, you’re a good reader you made it to here so you gotta want to get a Big Book on Migraine. Check this out.