Are Migraine and Panic Disorder Related? 2023
Migraine is a genetically inherited, neurobiological illness consisting of moderate to severe one-sided, throbbing headaches that come with sensitivity to light and noise and nausea and vomiting. Migraine is very disabling, and more frequently occurs in women where it relates to estrogen, and less often occurs in men. 25% of women and 6% of men have migraine.
Get started right. Read my article on “What is Migraine?” on my website, www.doctormigraine.com.
Panic disorder is one of the frequently occurring anxiety disorders that causes sudden, frightful attacks of physical and anxious symptoms that come out of the blue for no reason and are usually the subject of considerable worry in persons who have them.
Panic attacks come with sudden intense fear that usually comes with prominent palpitations and shortness of breath and the attacks often come out of the blue and also with severe headache for no reason so the patient often goes to the ER worried they may be experiencing a heart attack or a stroke.
Read my article, “Panic Disorder Symptoms” on my website, www.doctormigraine.com.
The question is whether these two dramatic medical problems relate to each other or come together? Panic attacks are distinguished from other forms of anxiety by their intensity and their sudden, episodic nature, but migraine is also episode and sudden in occurrence.
This is an article by Britt Talley Daniel MD, member of the American Academy of Neurology, the American Headache Society, migraine textbook author, podcaster, YouTube video producer, and blogger.
Panic disorder is a mental, anxiety disorder characterized by reoccurring unexpected panic attacks. Panic attacks are sudden periods of intense fear that may include rapid heart beat, palpitations, sweating, shaking, shortness of breath, numbness, or a feeling that something terrible is going to happen.
Migraine and Panic Disorder are 40% Comorbid, a term that means that these two conditions come together more commonly than chance. Many patients have the simultaneous occurrence of a migraine with panic symptoms and then report to the emergency room. This is not a rare problem and is called “panic migraine.”
Often times at the ER the headache portion of the patient’s history is paid attention to more than the panic symptoms and the patient is usually given a CAT scan which with migraine should be normal and then reassured that nothing is wrong.
For cardiac symptoms such as a racing heart or chest pain the patient is usually referred from the ER to see a cardiologist and for the headache, a neurologist.
Healthcare workers seeing such patients are strongly advised to review with the patient the 13 panic symptoms discussed below to make a diagnosis of a panic attack.
One attack of panic symptoms is called “panic attack,” but more attacks after that are referred to as “panic disorder.”
Get my Mini eBook on Migraine here.
Related questions.
Nosology
Migraine. Galen (131-201 A.D.) came from Pergamon in Asia Minor, an early center of learning and civilization. As a descriptive and diagnostic term, he offered “Hemicrania,” which means half of head, to describe one sided, sick headaches.
Eventually the “He” part of Hemicrania was deleted and the “micrania” part of the word was used.
Later Romans changed “Hemicrania” into the Latin “Hemicranium." The term later changed to “Hemigranea” which then became with successive translations and mistranslations “Migranea,” “Migrainea”, “Migrana,” and “Migrim” which is the term Liveing, the savant and great cataloguer of all things migraine, used in is famous text “On Megrim” published in 1873.
Later the French changed the word to its current and most popular form—“Migraine.”
Before the publication of the International Classification of Headache Disorders in 1988, the current accepted term, Migraine without aura was called “Common Migraine” and Migraine with aura was referred to as “Classical Migraine.”
Many patients even today still believe that if they do not have a typical visual aura such as spots or holes in vision, seeing half of things, or shimmery zig-zag lines, with headache that they do not have real Migraine.
Panic. Pan, in ancient Greek religion and mythology, was the god of the forest, of the wild, and of the shepherds. He was the god of fear and or lust. He played a pipe flute and was the companion of nymphs. His name comes from “paein,” meaning “to pasture.”
He had the hindquarters, legs, and horns of a goat which made him look satanic or like a faun or satyr. He was thought to be the god of fields, groves, and wooded glens and because of this became associated with fertility and the season of spring.
He usually has a beastly appearance with his goat horns, large muscular body, chest, and upper arms, and his goat like haunches, legs, and cloven feet.
Pan was always depicted as lusting after women.
A cloven foot is a split, hard, bony hoof like that of a horse or a goat which has traditionally been associated with the foot of Satan.
Pan and Daphne
The word “panic,” stressed initially the intensity of a feeling of fear, similar to the reaction provoked, according to the mythology, by the intervention of the God of the forest, Pan.
Currently panic refers to the anxiety state syndrome of Panic attack and Panic disorder, symptoms characterized by paroxysmal anxiety.
In the nineteenth century the English writer, James Barrie, changed Pan into a harmless spirit called Peter Pan who flew into Wendy’s room and took her to see the Lost Boys in Never never land, which was located the first star to the left and straight on till morning.
In the 1950’s this story was made into a cartoon movie by Disney studios, replete with songs and the evil Captain Hook striking at Peter with his hooked hand which had been bitten off by a crocodile.
The Fifth Diagnostic and Statistical Manual of the American Psychiatric Association (APA) is the APA’s universal authority for psychiatric diagnosis and impacts treatment advice and insurance payment by health care providers.
Panic disorder did not make it into the DSM until the 3rd edition, published in 1980. Medical school graduates before 1970 were likely not taught anything about panic attacks in psychiatric lectures or on rounds.
Pathophysiology
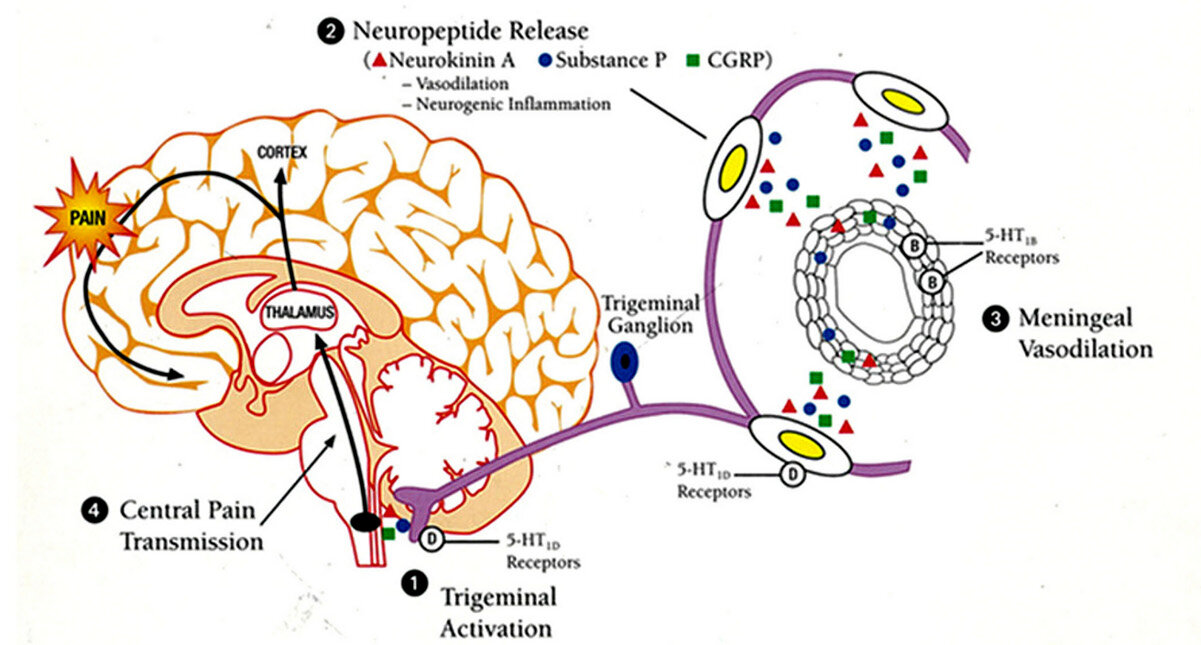
Migraine is a complex neurovascular process occurring in the central nervous system whereby the ganglia of the fifth cranial nerve, the Trigeminal nerve, and the cerebral arteries are activated and release three neurochemicals: Neurokinin A, Substance P, and Calcitonin Gene-related Peptide (CGRP).
These neurochemicals inflame the trigeminal nerve, the arteries, and the pain center of the brain, the thalamus.
The Migraine Timing Cycle
1. Trigeminal activation. The fifth cranial nerve, the sensory nerve of the face, is turned on by the migraine process causing pain to come to the eye, forehead, face, sinus, back of neck, and jaw.
2. 20-40 minutes later the neurochemicals CGRP, Neurokinin A, and Substance P are released by the migraine process from ganglia to inflame the trigeminal nerve, the arteries, and later the thalamus.
3. At 2 hours the arteries vasodilate and are inflamed. Blood pulsing through dilated, inflamed arteries causes pulsatile, pounding headache.
4. Past 3 hours the thalamus, also known as the pain center of the brain is turned on by the migraine process.
The Migraine Timing Cycle
If I drop a brick on my foot, the tissue of the foot is damaged and the pain is carried by pain nerves in the foot to the leg, to the spinal cord, and up to the thalamus in the brain where pain is registered. Migraine is a chemical inflammatory condition affecting the 5th nerve, the arteries, and thalamus.
Phase 4 is also called central sensitization, and this is the worst and most painful part of a migraine. During central sensitization touch may be perceived as painful, so the head is sensitive to touch or wear glasses or lie on one side in the bed. This is called allodynia, a sure clinical sign of central sensitization. Central sensitization is like sunburn. Normally it does not hurt to touch my arm, but if it does if it is sunburned. Sunburn is like allodynia.
Panic Disorder activates the sympathetic nervous system, which is part of the autonomic nervous system. The autonomic nervous system controls functions of the body so that one does not have to think to produce the reaction, the system kicks in automatically and without any conscious effort. Common functions that the autonomic nervous system controls are pupillary dilation (in a dark room) and constriction (in bright light.)
An emotional response such as sadness can cause the lachrymal glands in the lateral portions of each eye to secrete tears. Thinking about, seeing, and smelling food causes the salivary glands to secrete saliva. Imagine what it would be like to eat a cracker, a rather hard, dry substance, without salivation.
And so, peristalsis, monitoring the blood pressure, the heart rate, sweating, urinating or having a bowel movement, and all the sexual organs are governed by the autonomic nervous system.
It is sort of like driving a car through an automatic car wash. The motor is off. The driver just sits there. The car slowly moves through a series of hoses that wash and then rinse the car. Finally, a great warm fan blows all the water off and the driver is outside again—with a clean car.
The autonomic nervous system has two divisions: the sympathetic, which stimulates various bodily actions, and the parasympathetic which inhibits them. Panic attacks turn on the fear circuit of the brain and the sympathetic nervous system which generates the fight or flight response.
The Fight or flight response
Both panic attacks and anxiety turn on the brain’s “fight or flight” mechanism. The patient may report an intense desire to flee from wherever the attack is occurring. Patients commonly arrive at an emergency room or other medical setting believing that their symptoms represent a heart attack, stroke, or some other catastrophic medical condition
Anatomy of the autonomic nervous system
Neurons or cell bodies of the autonomic nervous system are located in the brain or the spinal cord, which is the central nervous system, while the second nerve cell is located in autonomic ganglia which lie laterally on both sides of the body adjacent to the brain stem or spinal cord. The autonomic nervous system supplies the pupils, salivary, and digestive glands and also the stomach, intestine, liver, kidneys, bladder, genitals, lungs, heart, and skin.
Function of the autonomic nervous system.
The autonomic nervous system controls.
• Blood pressure
• Heart and breathing rates
• Body temperature
• Digestion
• Metabolism
• Fluid and electrolyte balance
• The production of body fluids such as saliva, sweat, tears
• Urination
• Defecation
• Sexual response
The two divisions sometimes have opposite effects on the same organ. The sympathetic division increases blood pressure while the parasympathetic system decreases it. The sympathetic nervous system hastens the pulse and contractibility of the heart. It dilates airways to facilitate breathing, releases stored energy, and increases muscular strength. The sympathetic nervous system causes the palms to sweat, the pupils to dilate, and goosebumps as hair follicles stand straight up.
The sympathetic nervous system slows function in body areas that are not as important in an emergency, such as digestion and urination.
The parasympathetic nervous system controls the body during ordinary, normal times. It slows the heart rate, decreases blood pressure, stimulates digestion to process food and eliminate waste, and stores energy from food to restore and build up the body.
The Sympathetic nervous system increases
Heart rate and force of heart contraction
Release of energy stored in the liver
Basal metabolic rate, the speed at which energy is used for body functions
Muscle strength
Widens the airway to make breathing easier
Causes sweaty palms
Causes the release of semen (ejaculation)
The Parasympathetic nervous system
Stimulates the digestive tract to process food and eliminate waste
Slows the heart rate
Reduces blood pressure
Controls erections
How symptoms of a panic attack relate to the autonomic nervous system:
Palpitations, pounding heart, or accelerated heart rate.
Sweating.
Trembling or shaking.
Sensations of shortness of breath or smothering.
Feelings of choking.
Chest pain or discomfort.
Nausea or abdominal distress.
Feeling dizzy, unsteady, light-headed, or faint.
Chills or heat sensations.
Paresthesias (numbness or tingling sensations).
Derealization (feelings of unreality) or depersonalization (detached from oneself).
Fear of losing control or “going crazy.”
Fear of dying.
Palpitations, sweating, and trembling come from sympathetic nervous system activation. Shortness of breath and dizzy, light-headedness, chill or a heat sensation come from the hyperventilation and the exchange of blood gases that prevails during a panic attack.
Choking and chest pain likely come from smooth muscle activation via the sympathetic nervous system. Nausea comes from vagal nerve activation causing gastric acid secretion while derealization, fear of losing control, and fear of dying are pure psychiatric sensations without autonomic involvement.
Definition of Migraine without aura according to the International Classification of Headache Disorders 3rd edition (ICHD3).
Description:
Recurrent headache disorder manifesting in attacks lasting 4-72 hours. Typical characteristics of the headache are unilateral location, pulsating quality, moderate or severe intensity, aggravation by routine physical activity and association with nausea and/or photophobia and phonophobia.
Diagnostic criteria:
A. At least five attacks fulfilling criteria B-D
B. Headache attacks lasting 4-72 hours (untreated or unsuccessfully treated)
C. Headache has at least two of the following four characteristics:
1. unilateral location
2. pulsating quality
3. moderate or severe pain intensity
4. aggravation by or causing avoidance of routine physical activity (e.g., walking or climbing stairs)
D. During headache at least one of the following:
nausea and/or vomiting
photophobia and phonophobia
Not better accounted for by another ICHD-3 diagnosis.
DSM5 Diagnostic Criteria of Panic Disorder.
Patients experience unexpected attacks with an abrupt surge of intense fear or intense discomfort that reaches a peak within minutes, and during which time four (or more) of the following symptoms occur:
Palpitations, pounding heart, or accelerated heart rate.
Sweating.
Trembling or shaking.
Sensations of shortness of breath or smothering.
Feelings of choking.
Chest pain or discomfort.
Nausea or abdominal distress.
Feeling dizzy, unsteady, light-headed, or faint.
Chills or heat sensations.
Paresthesias (numbness or tingling sensations).
Derealization (feelings of unreality) or depersonalization (feeling detached).
Fear of losing control or “going crazy.”
Fear of dying.
Culture-specific symptoms (e.g., tinnitus, neck soreness, headache, uncontrollable screaming or crying) may be seen. Such symptoms should not count as one of the four required symptoms. At least one of the attacks has been followed by 1 month or more of one or both of the following:
Persistent concern or worry about additional panic attacks or their consequences (e.g., losing control, having a heart attack, “going crazy”).
A significant maladaptive change in behavior related to the attacks (e.g., behavior designed to avoid having panic attacks, such as avoidance of exercise or unfamiliar situations).
Panic attacks may become associated with a variety of situations in which patients feel an attack is more likely to occur, from which they would be unable to flee or get help quickly if an attack occurred, or in which they might be embarrassed if others should notice they are having an attack.
In reality, a panic attack is often not apparent to an observer, which is why a patient can successfully disguise his condition from others. The development of agoraphobia (fear of being in crowds or around other people) is common and is defined as fear of places or situations in which the patient feels ”trapped.” Patients may not have thought through why they fear or avoid situations when they initially present for treatment. As a result of this fear, they restrict travel or need a companion to enter phobic situations, like going for medical examination with a new doctor.
Panic Disorder Diagnostic Features
A diagnosis of Panic disorder requires recurrent (more than one) unexpected panic attacks. Unexpected means a panic attack for which there is no obvious cue or trigger at the time of the occurrence—that is, the attack appears to occur from out of the blue, such as when the individual is relaxing or emerging from sleep (nocturnal panic attack).
In contrast, expected panic attacks are attacks for which there is an obvious cue or trigger, such as a situation in which panic attacks typically occur. Multiple attacks of different intensities may occur over several hours, which might feel as if one panic attack is rolling into the next, like waves. The sympathetic nervous system is activated during the panic symptoms.
In the United States and Europe approximately one-half of individuals with panic disorder have both expected and unexpected panic attacks. The frequency and severity of attacks vary widely from moderately frequent attacks such as one per week for months or more frequent attacks such as one every day for a week or so.
Attacks may come with four or more symptoms or sometimes less than four and the symptoms with attacks may vary from one to the next.
Worries about panic attacks usually relate to physical concerns such as worry that panic attacks reflect the presence of life-threatening illness such as heart disease or epilepsy. Affected individuals may have social concerns of embarrassment or fear of negative impressions from others because of visible panic symptoms.
Agoraphobia As a result of the panic symptoms and recurrent unexpected attacks, affected individuals may develop maladaptive behavior changes that often accelerate the attacks, such as restricting daily activities and avoiding panic inducing places or relationships, like leaving home, using public transportation, or shopping. These restrictions may lead to agoraphobia which consists of marked, intense, fear or anxiety triggered by real or anticipated exposure to a wide range of social situations. The patient stays home and does not like to leave.
Epidemiology
Migraine is an extremely disabling condition and first in frequency of all disabling neurological diseases.
Almost 3 % of worldwide disability attributable to a specific disease, in terms of years lived with a disability, is due to migraine.
Twenty-five % of women and 6% of men have migraine.
The overall prevalence of migraine is 12%.
40 to 50% of Americans living with migraine also have anxiety.
Persons with migraine may be up to 5 times more likely to have anxiety than persons who do not.
Migraine is a multifactorial disorder which links genetic, hormonal, environmental, dietary, sleep, and psychological aspects differently in each individual.
Migraine is a bio-behavioral disorder.
Panic Disorder Lifetime prevalence estimates are 22.7% for isolated panic attack without agoraphobia 0.8% for panic attack with agoraphobia but without panic disorder, 3.7% for panic disorder without agoraphobia, and 1.1% for panic disorder with agoraphobia.
An important finding is that many people have isolated panic attacks that do not meet the criteria for panic disorder. These people have elevated prevalence of other mental disorders, report greater general impairment, greater use of psychotropic medication, and psychiatric consultation. Panic attacks are thus viewed as fairly nonspecific risk markers for psychopathology. However, all epidemiological estimates are likely low because of the fact that although many patients with panic attack go to the ER or see a doctor, a clear diagnosis is very commonly not made because few ER medical providers go through all 13 panic attack symptoms to make a certain diagnosis.
Genetic link
Migraine is a complicated, genetically related, neurovascular disorder which clusters in families. Specific genes for hemiplegic migraine have been determined but for the usual occurring types of migraine, which are migraine without aura and migraine with aura, the best that can be said now is that migraine is a polygenic condition.
Panic Disorder Although the exact genetic structure that relates to panic disorder is unknown, certain genes are associated with the condition, making it occur more commonly in certain families. Of all the anxiety disorders, panic disorder has the strongest familial clustering and genetic relationships since half or more of persons with panic disorder have a family history of the disorder. Psychiatric disorders such as anxiety, depression and bipolar disorders are more common in parents of patients with panic disorder.
Sexual preference
Migraine affects 25% of women and 6% of men. Thus, women have migraine 3 times more than men. Migraine in the clinic is mainly a female problem.
The brain responds differently to environmental and internal signals that relate to development of neural systems. Hormonal fluctuations in women may alter the set point of migraine.
The cyclic changes of hormones may directly alter neuronal, glial and astrocyte function throughout the brain.
Estrogen is mainly excitatory and progesterone inhibitory on brain neuronal systems. These changes contribute to the migraine condition that most notably starts at puberty in girls.
Panic Disorder Women have a greater incidence of panic disorder than men. Studies show a 2:1 female to male ratio. Some studies suggest women also have more severe panic disorder than men and especially if they also have agoraphobia.
Women may have more respiratory, choking, feeling faint symptoms while men may have more sweating and stomach pain.
A theoretical consideration is that the female menstrual cycle with the periods of estrogen hormone dominance alternating with progesterone may have something to do with the increased incidence of panic disorder in women.
Progesterone metabolites have anxiolytic effects due to their agonistic effect on GABA/benzodiazepine receptors. Premenstrual dysphoric disorder may have a greater panic response in females.
Age affected
Migraine starts usually in the teens or early 20s. It is most common in the 30 to 40 age group. At least 90% of people with migraine experience a first attack before the age of 40.
Migraine generally improves with ageing, usually after age 50.
Panic Disorder. The median age for development of panic disorder in the United States is 20-24 years although a small number of cases begin in childhood. Onset after age 45 is rare.
Untreated the disorder consists of a chronic waxing and waning condition with some individuals having episodic attacks with years of remission and others experiencing severe continuous illness. A minority of patients have remission without relapses within a few years of onset.
Duration of attack
Migraine A single migraine attack by definition lasts 4-72 hours. This time element gets confusing with overtreatment with pain killers or headache medicine which may lead into medication overuse headache and chronic migraine so that headaches occur every day, or very frequently.
For migraine without aura the typical onset to peak for an attack is 30-120 minutes. For patients with migraine with aura, the headache usually comes in 5-20 minutes after the aura. Some aura migraine patients experience their aura in the middle or the end of their migraine headache.
Nocturnal wake up headaches start during sleep, but the patient may wake with the attack already at its peak.
Occasional migraine patients will have a very quick and intense headache that goes from 0 to 10 in 5 minutes or so and these patients should be offered the option to treat that headache with subcutaneous sumatriptan which works in 10 minutes as opposed to a sumatriptan tablet that works in 30 minutes.
Panic Disorder For patients with episodic panic attacks, the onset to the maximum number of symptoms occurs within minutes. A single panic attack usually lasts for 30 minutes but the duration can vary from seconds to hours.
Patients with chronic panic disorder may have continuous or half a day or hours of lasting symptoms that may come in revolving waves of intensity.
Specific panic symptoms may change from attack to attack, starting with rapid heartbeat and trouble breathing with one attack and then with numbness and tingling and dizziness with the next.
Neurologic workup
Patients with migraine or panic disorder need to have medical tests to rule out possible medical conditions.
A normal MRI scan of the brain with and without contrast will usually eliminate concerning brain disease and can be very reassuring to the anxious migraine panic patient.
Blood work such as a CBC, sed rate, urine analysis, thyroid panel, and electrolytes should be done.
Electrocardiogram (ECG), cardiology and neurologic consultations complete the workup.
Differential Diagnosis
Migraine should be differentiated from Tension-Type Headache, Acute Rhinosinusitis, or organic brain disease such as a tumor by the history and work up.
Panic Disorder
The differential diagnosis of panic disorder is large and includes:
Acute coronary syndrome
Acute pericarditis
Acute respiratory distress syndrome
Angina and myocardial infarction (dyspnea, chest pain, palpitations, diaphoresis)
Asthma (dyspnea, wheezing)
Atrial fibrillation
Atrial flutter
Carcinoid
Cardiac dysrhythmias (palpitations, dyspnea, syncope)
Chronic obstructive pulmonary disease
Congestive failure
Cushing disease
Embolism
Fibromyalgia
Heart failure
Huntington disease
Hyperthyroidism (palpitations, diaphoresis, tachycardia, heat intolerance)
Hypoglycemia
Hypoparathyroidism (muscle cramps, paresthesiae)
Hyperparathyroidism
Illegal drugs (marijuana, cocaine, amphetamines)
Insulinoma
Meniere’s disease
Mitral valve prolapse
Migraine
Multiple sclerosis
Personality disorder
Pheochromocytoma (headache, diaphoresis, hypertension)
Porphyria
Premenstrual dysphoric disorder
Pulmonary embolus (dyspnea, hyperpnea, chest pain)
Multifocal atrial tachycardia
Schizophrenia
Seizure disorder (trembling and shaking, zoned out)
Pseudoseizure
Substance abuse/use—alcohol/sedative withdrawal, antidepressants, marijuana, caffeine, cocaine, amphetamines, methylphenidate, steroids, pseudoephedrine, mescaline, hallucinogen-LSD
Supraventricular tachycardia
Transient ischemic attacks, TIAs (unilateral paresthesiae)
Vestibular disorder, vertigo
Wilson disease
Withdrawal from CNS depressants (alcohol, barbiturates)
Typical case histories
Migraine New case
A twenty-five-year-old single woman presented with the chief complaint of “daily headaches for the past 30 days.” She has a previous history of allergies and depression and currently is on treatment with Zoloft.
She had a progesterone implant in her arm for contraception. She started having migraines at 12 years old at the same time she started her menstrual cycles (menarche).
She reports that the time her usual migraine lasts is 7 days. Using the International Classification of Headache Disorders (ICHD) check list for diagnosing migraine she had all the features of migraine without aura except nausea.
The ICHD check list is:
Migraine without aura
At least 5 attacks fulfilling criteria B-D
Headache attacks last 4-72 hours (treated or untreated)
Headache has at least 2 of the following 4 characteristics:
Unilateral, one sided, hemicrania, half of head
Throbbing, pulsating quality
Moderate or severe pain intensity
Aggravation by or causing avoidance of routine physical activity
During headache at least one of the following:
Nausea and/or vomiting
Photophobia and phonophobia
Her usual headaches are level 7-10 and usually right sided and throbbing. ICHD states that migraine headaches may be 5-10 while the other frequent type of headache, tension type headache, can only go from 1-5 and is a mild or moderate headache, while migraine headaches may be severe. Many patients answer “20” when asked to rate headache on a scale of 1-10.
This patient also carries chronic tension in her neck and shoulders which is a feature of generalized anxiety disorder (GAD.)
Neurochemicals are released by ganglia in the brain during a migraine and these chemicals are inflammatory, like applying acid to the back of your hand, and cause dilatation of the cerebral arteries. When blood from the heart pulses through this inflamed and dilated artery, it causes the artery to stretch and that hurts, resulting in a “throbbing or pulsating” headache. According to ICHD tension type headache is described as “pressure or tight” and is a bland, featureless headache.
Migraine headaches are usually one sided and come from the word hemicrania, an early term for migraine dating back to the Roman physician Galen in 235. Taking off the letters ‘he’ from hemicrania leaves the word ‘micrania’ from which migraine comes. There is no known reason why migraine headaches are one sided, but it is a secure clinical feature. Many patients say that their headaches are always “side locked” to just one side rather than switching sides, coming on the right side most of the time but occasionally coming on the left.
Considering organic or “serious” symptoms of headache, a headache that switches from side to side is just what migraine does, but a diseased artery with an aneurysm or arteriovenous malformation may always give the same one-sided headache. So, a migraine headache that switches from side to side is a reassuring and benign feature.
She also has menstrual headaches (defined as a migraine that starts the day of bleeding with the menstrual cycle or two days before bleeding or two days after starting to bleed), nocturnal headaches, and wake up headaches. Most all menstrual headaches relate to migraine and menstrual headaches start 3 weeks into the usual 30-day cycle when bleeding occurs and the internal estrogen level drops.
Nocturnal headache has a wide differential diagnosis of other headache causes including subarachnoid hemorrhage from intracerebral aneurysmal rupture, temporal arteritis, cluster headache, hypnic headache, or a brain tumor. However, the most frequent cause of nocturnal headache is migraine.
The neurochemicals that come out during migraine make the patient very sensitive to movement or being up, so the typical patient wants to lie down quietly or try to go to sleep, which will sometimes result in the patient awakening several hours later feeling better. Cluster type headache patients have to be up and moving, and they may pace around the room.
The human brain has a trigger zone for nausea and vomiting in the upper medulla which may be turned on by the migraine process. This is why migraine may be called “sick headache.”
The migraine process inflames and irritates the sensory cranial nerves and so hearing, carried by the eighth acoustic nerve may be inflamed so that mild noises are felt in the head as painful and the patient has “sonophobia.”
Likewise, the retinal neurons in the eye are inflamed so that light coming into the eye is painful and the patient reflexly closes his eyes and has “photophobia.”
ICHD does not list allergy as a causation of headache so there really is no “allergic headache.” But depression is linked to migraine about 50% of the time along with generalized anxiety disorder (GAD) 40 % of the time.
The case study we started with had a history of depression and menstrual headache. These may be called migraine “links” which are associated features of migraine that alone are not diagnostic but with a positive ICHD check list present a comprehensive view the totality of the migraine syndrome.
During sleep there are usually 3 or 4 dream events spread out through the night during which time the eyes rapidly move, and this feature can easily be detected during an EEG, electroencephalogram, by recording electrodes places near the eyes. During dreaming the internal autonomic system turns on and the cerebral arteries go into vasospasm, which then is released at the end of the dream state so that the patient may “wake up at the end of a dream” with a bad migraine. These come deep in the night or many times about 2 hours after wakening in the morning.
For a person who went to sleep at 11 p.m. and usually awakens at 7 a.m., the last dream event may come at 5:30 a.m. The problem is that many patients do not wake up at the start of the migraine and are not able to treat early, like with one of the triptan drugs which should be taken early in the migraine process. Sleep continues and the migraine process goes on, the chemicals are released, and then the patient has a severe “wake up” headache which is hard to treat. This patient started with a wake-up headache 30 days before I saw her. Such a headache may start a process of taking too much medication which then keeps the headaches coming.
The patient also mentioned that her usual migraine lasted 7 days. This amount of time is not consistent with the ICHD concept which gives a strict time duration for an episode of migraine that can only last 4-72 hours. So, an episode of migraine could last 3 days but not 7 days.
This patient had already had a normal CAT scan of sinuses and MRI brain scan when I met her, and she had a normal neurologic exam. With these reassuring features I could be very certain that she was over treating with analgesics and getting medication overuse headache and likely short-term chronic migraine (defined as 15 headache days a month, 8 of which have migraine features.) On close inquiry she admitted to the following medications which she rotated:
No caffeine
Tylenol (acetaminophen) 500 mg for the past 2 weeks every day 2-3 tabs
Fioricet (acetaminophen, caffeine, butalbital) the past 3 days 2/day
Sumatriptan 100 mg for the past 3 days 1/day
Tramadol for 2 days 1/day
Only 3-4 percent of the world population get medication overuse headache although the incidence of migraine peaks in women at age 42 so that 25% of women have migraine at that age. Not all migraine patients get medication overuse headache and it may be a special genetic feature of certain migraine patients which has not been defined yet. In general migraine patients should limit caffeine and over the counters and triptans and narcotics to no more than 2 days a week and they will probably stay free of medication overuse headache.
Read my handout on the webpage about the migraine lifestyle and medication overuse headache to get up to date with those subjects. The day I saw this patient I advised her to stop all painkillers, triptans, and narcotics (tramadol, Fioricet).
I asked her to do the migraine lifestyle, start a preventive drug, amitriptyline 10 mg at night, to continue her Zoloft, to take a week of prednisone 20 mg three times a day for 7 days, and to use Migranal generic DHE nasal spray 2-4 sniffs as needed every 4 to 6 hours. I asked her to call me for problems and to return to clinic in 7 days.
Long range she might consider use of one of the CGRP preventive drugs like Aimovig. Hopefully, she will do well.
Panic Disorder
Clinical scenario
Bill left work after a stressful day and dropped into a bar he liked to attend. Then after a few beers and talk with the boys he found himself back in his car winding his way home through the evening traffic when all of a sudden his heart pounded so hard and fast that his chest started hurting and he broke out in a sweat. He felt dizzy and lightheaded, sick at his stomach, and then felt numbness and tingling in his left cheek and left hand. He could not get his breath. He pulled the car off the road and stopped in the parking lot of a strip shopping center.
He thought he might be dying and was reduced to terror, suddenly, without cause. Then, almost as quickly as the attack occurred, it faded away.
Thinking he had had a heart attack, Bill rushed to an emergency room, where he was examined and had a normal EKG, CAT scan of the head, and basic blood work. He was told “everything was all right” but could not understand what that could mean. How could he have experienced such symptoms with nothing being wrong. Bill doubted the doctor and the staff at the ER but was lightly reassured by the normal tests. He put it out of his mind and tried to forget about it but remembered the spell every time he sat down in his car to drive. What if, during another attack, he could not control the car and he inadvertently plunged into another car or a pedestrian on the road? The whole thing made him nervous.
But, several days later, he had another attack, and then others followed, and Bill started worrying a lot that he was losing control of his life and might even be going crazy. He started avoiding social activities like being around other people and developed moodiness, insomnia, and a low energy level. He became even more concerned about driving his car and kept trips to short distances. He pretty much quit going out, except for work and the grocery store. He quit exercising, even though he had already paid for a month at the gym. He just could not force himself into the car.
At this point, Bill’s world seemed to shrink and as he stayed in more and more and then felt he could not drive to work, so his bills piled up and he quit seeing friends and got depressed. Eventually, Bill was diagnosed as having panic disorder and his doctor explained that it resulted from an altered neurochemical imbalance in the brain which triggered attacks like he had been having. The doctor reassured Bill the attacks were not a sign of mental weakness or personal failure. Instead, they were a sign that the body’s alarm mechanism, which prepares us to fight or flight was out of order. The doctor assured Bill that even though his intense feelings of losing control or dying could be overwhelming or frightening that no one had ever died from a panic attack. After a period of treatment with medication and psychological therapy, Bill now lives a more normal life.
Anxiety vs. panic attack
Everyday people like Bill are rushed into emergency rooms with symptoms that might indicate anything from heart disease to asthma. About a third of the time, what they are experiencing is a panic attack—an unprovoked explosion of bodily sensations and fear. It has been shown that most panic disorder patients consult physicians other than psychiatrists 10 or more times before their condition is accurately diagnosed.
A panic attack is characterized by sudden, brief episodes of physical and mental symptoms which, by definition, occur spontaneously or “out of the blue,” to differentiate it from anxiety attacks that have never occurred spontaneously and have always been secondary to a specific reason.
For anxiety attacks the patient should have insight or a reason as to why the event occurred. For example, anxiety would come after a sudden attack with a knife by an assailant who wanted to kill you. There would be an evident reason for the symptoms resulting from such an attack.
This is not true with panic attacks which generally are unprovoked, leaving the victim uncertain where all the symptoms came from. Although panic attacks can also come after stressful events, the majority of them come for no reason. With concomitant fear and agoraphobic avoidance of interaction, repetitive panic attacks can lead to panic disorder.
Because true, organic seizure and pseudoseizure are commonly in the differential diagnosis of panic disorder symptoms, these 2 medical entities are described in detail here.
Seizure vs. panic attack
A quite common neurologic problem is differentiating a true organic epileptic seizure from a panic attack. The two medical problems may occur together or separately alone. Panic attacks may cause trembling or shaking while epilepsy movements are usually called jerking or twitching although panic attack patients with hyperventilation may have small widespread twitching of muscle, called fasciculation which is confusing, and the twitching may imitate true minor motor seizures.
As always in medicine, a history from a second person witness is important to obtain and may/may not be helpful. Panic attack patients may experience depersonalization or derealization which is an altered level of consciousness where they may be “zoned out” which can imitate absence or partial complex seizures. Fear associated with some partial complex epileptic seizures can be confused with the “fear of dying” symptom of panic attack.
The situation is that true organic epilepsy usually does not have palpitations, a rapid heartbeat, shortness of breath, chest tightness, fear of losing control, or fear of going crazy.
The examiner has to think differentially between panic and epileptic events and ask questions that would separate these two problems. The examiner should always ask the cardinal 13 panic attack defining symptoms and add them up with a check list.
Panic attack patients may black out or faint and fall and possibly hurt themselves or bump their head, whereas true unexpected seizure patients may fall hard and split their scalp, needing stitches.
The list of partial complex seizure symptoms should also be reviewed with questions asking about a “rising sensation from the stomach up into the head,” a bad or unusual smell or taste, or occurrence of the Deja Vue or Jamais Vue phenomenon.
And it goes true to say usually without fail that patients who bite their tongue hard with incisional tongue lesions, present with bleeding scalp cuts that need stitches, urinary or fecal incontinence, a herald cry and then observed tonic/clonic jerking followed by foaming at the mouth, an ictus of 5-10 minutes, and confusion on recovery, are usually not having a panic attack. These patients are experiencing an epileptic seizure.
EEG monitoring is the ultimate litmus test here and a patient with an event associated with EEG monitoring of spike or sharp wave activity usually truly defines an epileptic seizure. The problem with this is how much monitoring should one do—a simple 30-minute outpatient EEG, 24 or 72-hour outpatient monitoring, or a week in the EEG unit? Insurance coverage and patient acceptance factor into this sort of a workup.
Psychogenic non-epileptic seizures (PNES) vs. panic attack
PNES are non-epileptic events which may resemble an epileptic seizure without the electrical discharges found with epilepsy. Patients with PNES may or may not have obvious psychological clinical symptoms. Approximately 30% of patients seen at specialist epilepsy clinics have PNES.
The symptoms of PNES are not definite and often mimic seizures. There may be vague thrashing, non-organic trembling and shaking, pelvic thrusting, or arc de cercle, in which the patient may arch their body backward until their shoulders approach their heels. PENS patients may bite the tip of the tongue, which is rare in epilepsy. They may have motor movement or jerking lasting more than 2 minutes. They may close their eyes during their spells or move their head from side to side. PNES patients resist forceful eye opening during the spell or when lying on a gurney unconscious may voluntarily control their arm so that it does not hit their own face when dropped by an examiner.
There is usually a strong psychogenic pattern to these patients with associated conversion reaction. The differential diagnosis includes syncope, stroke, frontal lobe seizures, factitious disorder (simulating seizures intentionally for psychological reasons), or malingering (simulating seizures for secondary gain such as compensation or avoidance of civil or criminal legal punishment.)
The best way to distinguish epilepsy from PNES is long term video-EEG monitoring with the aim of capturing one or two episodes with digital photography and simultaneous EEG monitoring which should be, at the time of the event, normal.
PNES may also be called non-epileptic attack disorder, functional seizures, psychogenic non-epileptic seizures, or pseudoseizures.
Prognosis
Prognosis is directly related to patient compliance and appropriate medical treatment.
Migraine now has a number of very competent acute therapy and chronic treatment options that patients may pursue.
Treatment with triptans, such as sumatriptan, at onset of a migraine produces a pain free state for 80% in 2 hours.
The new CGRP drugs for migraine prevention, such as Aimovig, which is delivered by subcutaneous injection once a month can reduce migraine attacks to 50% in half of patients, 75% in a quarter of patients, and 100% in another quarter.
Panic disorder may be treated by psychiatric consultation and the judicious as needed, short term use of one of the benzodiazepine drugs such as Xanax or Klonopin.
The patient may be treated with one of the Selective Serotonin Receptor inhibitors, such as Lexapro, given for chronic treatment as one a day.
The patient should be instructed in and do Cognitive Behavioral Therapy (CBT) which is a non-drug treatment helpful for anxiety.
This site is owned and operated by Internet School LLC, a limited liability company headquartered in Dallas, Texas, USA. Internet School LLC is a participant in the Amazon Services LLC Associates Program, an affiliate advertising program designed to provide a means for sites to earn advertising fees by advertising and linking to Amazon.com. Although this site provides information about various medical conditions, the reader is directed to his own treating physician for medical treatment.
All the best.
Follow me at: www.doctormigraine.com, Pinterest, Amazon books, Podbean, and YouTube.
Britt Talley Daniel MD